By Rose Meltzer, Fierce Healthcare | August 29, 2018
There’s a lot of buzz about digital health these days. Some say the latest high-tech tools have the potential to revolutionize not only healthcare, but health itself.
But what consumers actually want to use—or are able to use—is sometimes overlooked.
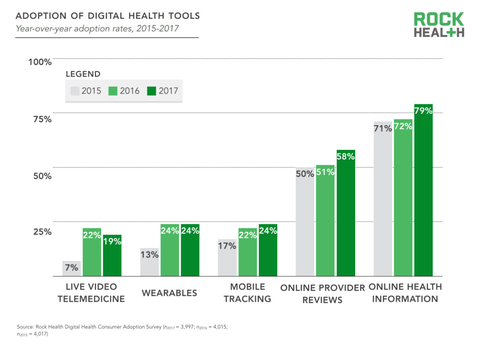
Now in its third year, Rock Health’s consumer survey asked 4,000 consumers about their digital health habits. Nearly 8 in 10 (79%) of those surveyed this year said they search for health information on the internet, and nearly 6 in 10 (58%) said they read online provider reviews.
Uptake among more promising technologies has been slower. Only a quarter (24%) reported using wearables or mobile apps to track their health, and just 19% use live video telemedicine (i.e. talking to a provider via video call).
Further, those who might benefit from these innovations the most, such as low-income individuals and chronically-ill seniors, use them the least.
Megan Zweig, who led the study, interpreted this discrepancy from a cost perspective.
“We all know how to use Google, so that information is at patients’ fingertips,” she explained. Tools like wearables, on the other hand, can be costly.
RELATED: Study shows wearables lack clinical impact, but researchers haven’t lost hope
But those patients are nevertheless “showing an appetite to use that information to inform their care decisions,” Zweig said. The survey also found that many of those patients track their health data and goals by memory or in a written journal.
Several insurers now offer patients discounted (or free) activity trackers, but Zweig noted patients may not know those offers exist.
“That knowledge gap can be a big impediment,” she said, adding that payers should “make known what services are available and what the costs are.”
The key to increasing use of wearables is “not necessarily…encouraging people that are already spending too much out-of-pocket on healthcare to pay even more for these solutions,” Zweig said. Instead, payers, both public and private, should determine “the right reimbursement pathway.”
RELATED: CMS physician payment proposal nudges open the door for telehealth
Meanwhile, the key to expanding telemedicine may be a bit old-fashioned.
“Relationships matter,” the survey says. Only 53% of live video telemedicine patients said they were satisfied with their virtual visit if they hadn’t met the provider in-person beforehand. But among patients who did know their provider in-person, that number leapt to 92%.
Zweig noted the potential in “asynchronous” telemedicine as well—for example, sending a provider a photo of an injury instead of arranging a time to talk about it.
But keeping patients healthy and satisfied while striving for value is critical, Zweig said.
“Even here at Rock Health, we spend a lot of our time tracking things like venture dollars and validation milestones of our portfolio companies and of the broader ecosystem. But at the end of the day, that doesn’t tell you much about how people are using these tools,” she said.

