The Medical Futurist | September 7, 2019
How do you study organs and complex living structures in two dimensions? It’s like trying to piece together life on the planet in the age of the dinosaurs from fossils – almost impossible. So why do medical schools require students to learn the tricks of the trade from densely written books and PowerPoint presentations? Luckily, the advancement of technology brought in another dimension: virtual reality. So, we looked around to what extent VR as a three-dimensional teaching tool can support medical education. Let’s dive into virtual laparoscopy, simulated empathy, and co.
Can simulated realities trick your senses?
In April, NATO conducted the largest military-medical exercise in the history of the Alliance in Romania. In one of the huge military containers called ‘virtual reality center’, paramedics sat in front of screens simulating building collapses, mass casualties, and environmental disasters, such as earthquakes, gas leakage, or radiation. The task was to coordinate their moves to see how they communicate with various units, soldiers, firefighters, first responders in difficult situations and how they make decisions.
While soldiers and by-standing journalists casually chatted about local food or which location to visit next, loud screams and clouds of dust indicated on the screen that a building just collapsed due to a strong earthquake – and tons of people need help. Although paramedics were visibly focused on the task, and completed what they were supposed to do, they were in a safe environment without the adrenalin rush and/or paralyzing fear that comes with dangerous disaster situations. On the other hand, they could perfect the skills needed to successfully coordinate the team in such scenarios to such an extent that they would come instinctively in live situations.
And although current virtual environments, which work by replacing users visual and aural connections to the real world with connections to a virtual environment through the use of headphones and a VR headset, perhaps cannot trick your brain into believing you are seeing a ‘real emergency situation’ as the visual and audio effects still reveal that its VR, that could soon change with the rapid transformation of the technology. Perhaps, in some years, we will rather be worried about VR mimicking reality to such an extent that soldiers or doctors could not even distinguish that from reality. Perhaps, developers may decide in the future that just as with creating robots that do not mimic human physiology on purpose, they will create ‘imperfect’ immersive environments so that users will know and feel that they are dealing with a ‘training set’.
While the problems around the distinction of simulation and reality might become louder with the perfection of technology, the rapid spread of virtual reality training around various professions shows that it fills a yawning void in educational practices. Let’s see some examples of how VR can make a difference for medical students.

Practicing on virtual dissecting tables and simulating diseases
Medical students have to learn by heart so much information and have to prepare for so many different situations with the help of such medieval means that its painful to even think about it. When you are studying anatomy from a 500-page-long book with black-and-white pictures and 10 pt font size, no one can seriously expect you to understand and learn it efficiently. How are you supposed to imagine the brain if you have never seen one? Or, if you feel sick in the dissection practice and cannot even look at the dead body in front of you?
These are the exact situations where VR offers a viable solution. The Anatomage Table is the world’s first virtual dissection surface perfect for teaching anatomy easily and spectacularly. The HoloLens mixed reality device is also a great tool for studying the human body, for example, through the use of the HoloHuman app.
Some universities already introduced or are in the process of implementing such new technologies. In collaboration with the Cleveland Clinic, Case Western University opened its new Health Education Campus, which is completely cadaver-free. Students from CWRU’s dental, medical and nursing schools will learn anatomy in realistic and transferable ways, through virtual and/or mixed reality devices. Using the HoloLens and CWRU-developed curriculum, medical students will learn anatomy by viewing 3D holograms of the entire body. They will be able to look inside organs from any angle and investigate how different diseases and injuries affect different body parts.
In Denmark, the medical community and regulators believe in the power of this new technology so much that they even introduced a new policy in the Capital Region that requires physicians in all specialties to complete a compulsory simulation-based training program – prior to progressing to live patient training. We believe that this practice could evolve into a general rule of thumb in medical education in the future.

Teaching empathy to medical students with virtual simulations
Surprisingly, another area where VR could make a difference is teaching empathy. Although medical students leaning over thick volumes of anatomy might not share this view at earlier stages of their studies, but one of the most challenging parts of being a doctor is mastering the patient-doctor communication. Empathy is an indispensable tool here.
Delivering difficult news being it about a cancer diagnosis or the death of the patient to the family requires enormous strength of mind and empathy from the doctor, but also appropriate practice. That is where VR comes into the picture. Researchers from Medical Cyberworlds Inc. and the University of Michigan conducted research with 421 medical students about the use of VR in patient-doctor communication. They used the Mpathic-VR technology that allowed users to talk with emotive, computer-based virtual humans who can see, hear and react to them in real-time. The virtual humans used a full range of behaviors expected of two people talking together. Applying this technique in future curriculums, med students could practice difficult conversations before going out and experiencing them in real life.
What it means to be Alfred or a patient suffering from schizophrenia
Another strand of virtual training uses that component of empathy when someone imagines another person’s state as if that happened to them. Dozens of companies are developing virtual reality environments where the user can experience how is it to live with a disability or a certain condition. For example, the interactive digital marketing company Viscira has deployed programs that mimic the symptoms of schizophrenia and macular degeneration. Excedrin’s “The Migraine Experience” marketing campaign for headache medicine simulates common migraine effects like light sensitivity, vision loss, and disorientation. Embodied Labs created “We Are Alfred” by using VR technology to show young medical students what aging means. Everyone can be the hypothetical Alfred for 7 minutes, and experience how it feels like to live as a 74-year-old man with audio-visual impairments.
Although more research is needed into the effectiveness of such virtual simulations in the long run, some studies suggest that they work. Participants who experienced a color-blindness simulation, for instance, were more likely to help real color-blind people. Similarly, those who completed a schizophrenia simulation and read about the condition had greater empathy than people who did the reading without the VR experience.
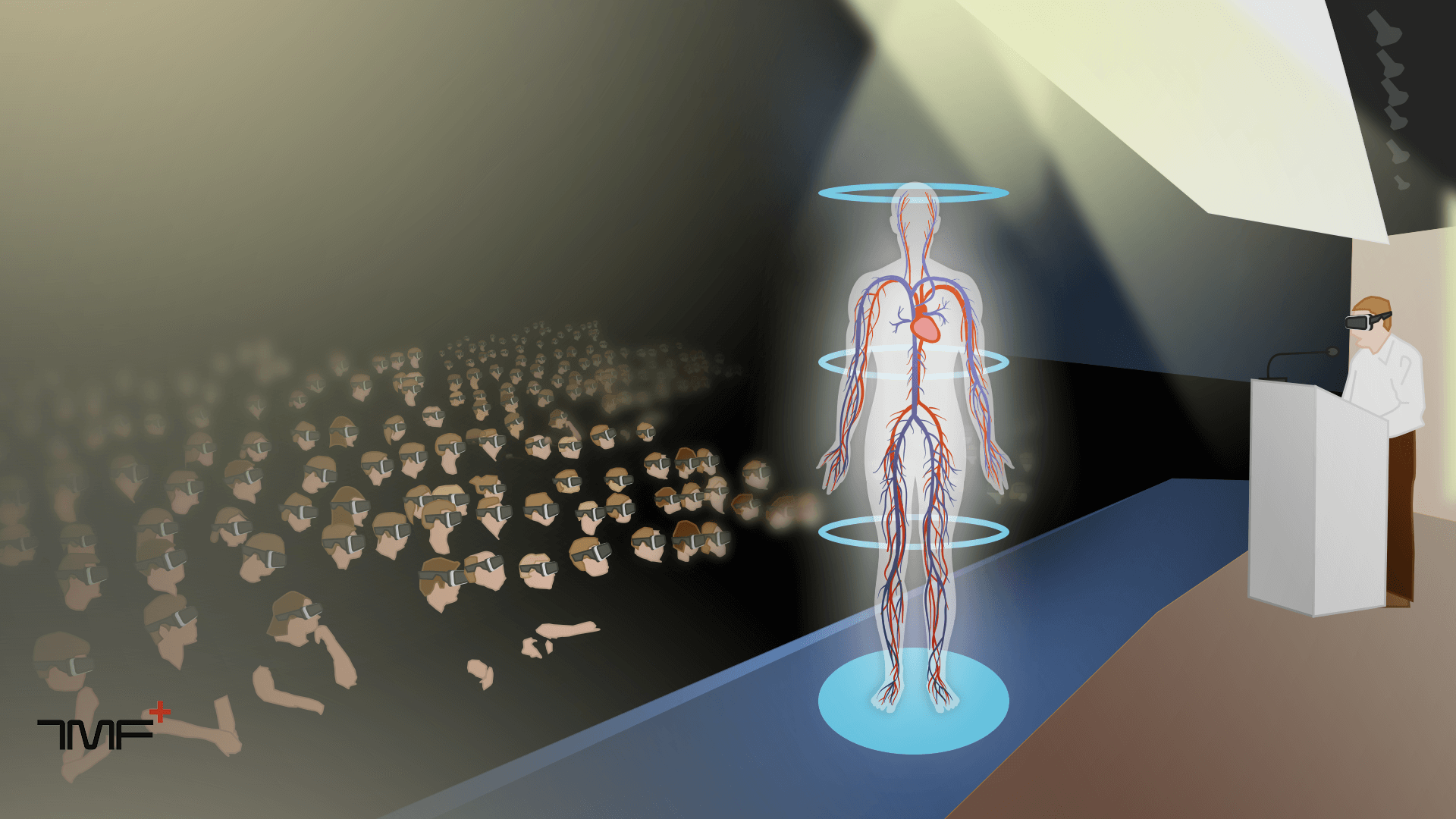
Virtual presentations for medical conferences
Soon it will not be enough for speakers either to get on the stage of scientific conferences with bullet-pointed PowerPoints when the world is immersing into 3D movies and life-like video games. VR could enhance the content of presentations and visualize ideas which are otherwise difficult to imagine. This is especially important in healthcare, where sometimes it is easier to point to a specific area in the human body than describe it.
Imagine an audience and the presenter wearing Oculus Rift or Sony Morpheusdevices, and a huge VR skull floating around on the stage. All the devices are connected and if you don’t have your headwear, you only see an empty stage. Expert of applying VR in medicine, Brennan Spiegel and his team already provided a similar experience. He told The Medical Futurist that with the help of Medscape and Confideo Labs at a #MedEd lecture he talked to his colleague, Dr. Lin Chang, who was in “real reality” on the stage, while Spiegel walked around in VR, interacting with the slides and engaging in a conversation about them with other colleagues. A live audience watched the scene all unfold. “I’m convinced this is the future of live stage CME talks. I will do this again and in full at the Virtual Medicine conference next March at Cedars-Sinai”, added Spiegel.
Training and retraining for practicing physicians
One of the most difficultly achievable criteria for medical professionals is to stay up to date all the time and have a sharp mind that’s able to pull out knowledge in the toughest emergency situations. Constant training and re-training could help nurses, doctors, and other practitioners in staying on top of their game – and VR could greatly support this effort.
For example, the Miami Children’s Hospital is using virtual technology to train employees on procedures such as cardiopulmonary resuscitation, nasal gastric tube insertion, starting an IV, wound care and others. They may use a similar platform as Virtual Education Systems’ VR training systems; new nurses can train with interactive patients in-hospital simulations making critical decisions in real-time.
Another company, Surgical Science, offers virtual simulations for laparoscopic interventions and endoscopic procedures – as they believe that laparoscopic skills come with repetition. Surgeons have several other solutions as well to maintain and improve their skills. ImmersiveTouch, for example, offers a VR imaging platform that allows surgeons to see, feel and experience minimally invasive surgical pathways to improve surgical precision and patient outcomes. Osso VR is working in the field of orthopedic surgeries and aims to improve the method of surgical training. A Cleveland-based company, Surgical Theater asked the question whether surgeons can be trained as fighter pilots able to pre-fly their missions – and they built an immersive environment just to provide the exact conditions for efficient surgical planning of operations.
In some places, VR became so critical in certain specialized medical training that no one can practice without mastering it. For example, since 2013, every doctor planning to specialize in orthopedics in Switzerland has had to pass an exam on a VirtaMed ArthroS simulator. Not only surgeons or nurses can benefit greatly from VR training settings. Residents and clinicians can double-check their diagnoses with the help of Human DX, or engage in a virtual environment for practicing how to solve cases more efficiently with the InSimu Patient App.
As you can see it’s a little bit like in chess: the best chess players solve dozens of chess problems every day so that they can be more skilled when they are playing for real. Virtual reality allows something similar for medical students, physicians, or nurses – to stay at the top of their game every single day. But it not only offers the broadening of cognitive knowledge but also how to bring people together. With its ability to show the experiences of others, it can teach empathy and connect humans in such profound ways that it was never thought before. Being able to experience aging, schizophrenia, or macular degeneration through the eyes of a virtual patient could be eye-opening. Thus, we agree completely with VR creator Chris Milk, who said in one of his TED talks that through VR “we become more compassionate, we become more empathetic, and we become more connected. And ultimately, we become more human.”

