By Jennifer Bresnick, Health IT Analytics | April 11, 2019
These twelve artificial intelligence innovations are expected to start impacting clinical care by the end of the decade.
There’s no question that artificial intelligence is moving quickly in the healthcare industry. Even just a few months ago, AI was still a dream for the next generation: something that would start to enter regular care delivery in a couple of decades – maybe ten or fifteen years for the most advanced health systems.
Even Partners HealthCare, the Boston-based giant on the very cutting edge of research and reform, set a ten-year timeframe for artificial intelligence during its 2018 World Medical Innovation Forum, identifying a dozen AI technologies that had the potential to revolutionize patient care within the decade.
But over the past twelve months, research has progressed so rapidly that Partners has blown up that timeline.
Instead of viewing AI as something still lingering on the distant horizon, this year’s Disruptive Dozen panel was tasked with assessing which AI innovations will be ready to fundamentally alter the delivery of care by 2020 – now less than a year away.
Sixty members of the Partners faculty participated in nominating and narrowing down the tools they think will have an almost immediate benefit for patients and providers, explained Erica Shenoy, MD, PhD, an infectious disease specialist at Massachusetts General Hospital (MGH).
READ MORE: Verma: Artificial Intelligence is Key for Patient Empowerment, Lower Costs
“These are innovations that have a strong potential to make significant advancement in the field, and they are also technologies that are pretty close to making it to market,” she said.
The results include everything from mental healthcare and clinical decision support to coding and communication, offering patients and their providers a more efficient, effective, and cost-conscious ecosystem for improving long-term outcomes.
In order from least to greatest potential impact, here are the twelve artificial intelligence innovations poised to become integral components of the next decade’s data-driven care delivery system.
NARROWING THE GAPS IN MENTAL HEALTHCARE
Nearly twenty percent of US patients struggle with a mental health disorder, yet treatment is often difficult to access and expensive to use regularly. Reducing barriers to access for mental and behavioral healthcare, especially during the opioid abuse crisis, requires a new approach to connecting patients with services.
AI-driven applications and therapy programs will be a significant part of the answer.
READ MORE: AI, Deep Learning Start to Tackle Common Problems in Healthcare
“The promise and potential for digital behavioral solutions and apps is enormous to address the gaps in mental healthcare in the US and across the world,” said David Ahern, PhD, a clinical psychologist at Brigham & Women’s Hospital (BWH).
Smartphone-based cognitive behavioral therapy and integrated group therapy are showing promise for treating conditions such as depression, eating disorders, and substance abuse.
While patients and providers need to be wary of commercially available applications that have not been rigorously validated and tested, more and more researchers are developing AI-based tools that have the backing of randomized clinical trials and are showing good results.

Source: Partners HealthCare
STREAMLINING WORKFLOWS WITH VOICE-FIRST TECHNOLOGY
Natural language processing is already a routine part of many behind-the-scenes clinical workflows, but voice-first tools are expected to make their way into the patient-provider encounter in a new way.
Smart speakers in the clinic are prepping to relieve clinicians of their EHR burdens, capturing free-form conversations and translating the content into structured documentation. Physicians and nurses will be able to collect and retrieve information more quickly while spending more time looking patients in the eye.
READ MORE: Data Scientists in High Demand for Healthcare Providers, Payers
Patients may benefit from similar technologies at home as the consumer market for virtual assistants continues to grow. With companies like Amazon achieving HIPAA compliance for their consumer-facing products, individuals may soon have more robust options for voice-first chronic disease management and patient engagement.
IDENTIFYING INDIVIDUALS AT HIGH RISK OF DOMESTIC VIOLENCE
Underreporting makes it difficult to know just how many people suffer from intimate partner violence (IPV), says Bharti Khurana, MD, an emergency radiologist at BWH. But the symptoms are often hiding in plain sight for radiologists.
Using artificial intelligence to flag worrisome injury patterns or mismatches between patient-reported histories and the types of fractures present on x-rays can alert providers to when an exploratory conversation is called for.
“As a radiologist, I’m very excited because this will enable me to provide even more value to the patient instead of simply evaluating their injuries. It’s a powerful tool for clinicians and social workers that will allow them to approach patients with confidence and with less worry about offending the patient or the spouse,” said Khurana.
REVOLUTIONIZING ACUTE STROKE CARE
Every second counts when a patient experiences a stroke. In far-flung regions of the United States and in the developing world, access to skilled stroke care can take hours, drastically increasing the likelihood of significant long-term disability or death.
Artificial intelligence has the potential to close the gaps in access to high-quality imaging studies that can identify the type of stroke and the location of the clot or bleed. Research teams are currently working on AI-driven tools that can automate the detection of stroke and support decision-making around the appropriate treatment for the individual’s needs.
In rural or low-resource care settings, these algorithms can compensate for the lack of a specialist on-site and ensure that every stroke patient has the best possible chance of treatment and recovery.
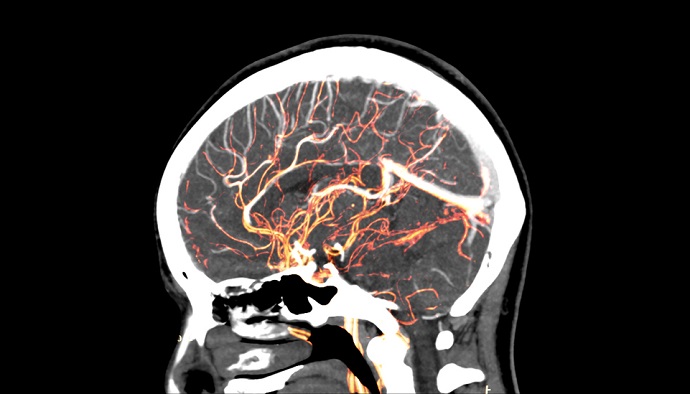
Source: Getty Images
REDUCING ADMINISTRATIVE BURDENS FOR PROVIDERS
The costs of healthcare administration are off the charts. Recent data from the Center for American progress states that providers spend about $282 billion per year on insurance and medical billing, and the burdens are only going to keep getting bigger.
Medical coding and billing is a perfect use case for natural language processing and machine learning. NLP is well-suited to translating free-text notes into standardized codes, which can move the task off the plates of physicians and reduce the time and effort spent on complying with convoluted regulations.
“The ultimate goal is to help reduce the complexity of the coding and billing process through automation, thereby reducing the number of mistakes – and, in turn, minimizing the need for such intense regulatory oversight,” Partners says.
NLP is already in relatively wide use for this task, and healthcare organizations are expected to continue adopting this strategy as a way to control costs and speed up their billing cycles.
UNLEASHING HEALTH DATA THROUGH INFORMATION EXCHANGE
AI will combine with another game-changing technology, known as FHIR, to unlock siloes of health data and support broader access to health information.
Patients, providers, and researchers will all benefit from a more fluid health information exchange environment, especially since artificial intelligence models are extremely data-hungry.
Stakeholders will need to pay close attention to maintaining the privacy and security of data as it moves across disparate systems, but the benefits have the potential to outweigh the risks.
“It completely depends on how everyone in the medical community advocates for, builds, and demands open interfaces and open business models,” said Samuel Aronson, Executive Director of IT at Partners Personalized Medicine.
“If we all row in the same direction, there’s a real possibility that we will see fundamental improvements to the healthcare system in 3 to 5 years.”
OFFERING NEW APPROACHES FOR EYE HEALTH AND DISEASE
Image-heavy disciplines have started to see early benefits from artificial intelligence since computers are particularly adept at analyzing patterns in pixels. Ophthalmology is one area that could see major changes as AI algorithms become more accurate and more robust.
From glaucoma to diabetic retinopathy, millions of patients experience diseases that can lead to irreversible vision loss every year. Employing AI for clinical decision support can extend access to eye health services in low-resource areas while giving human providers more accurate tools for catching diseases sooner.
REAL-TIME MONITORING OF BRAIN HEALTH
The brain is still the body’s most mysterious organ, but scientists and clinicians are making swift progress unlocking the secrets of cognitive function and neurological disease. Artificial intelligence is accelerating discovery by helping providers interpret the incredibly complex data that the brain produces.
From predicting seizures by reading EEG tests to identifying the beginnings of dementia earlier than any human, artificial intelligence is allowing providers to access more detailed, continuous measurements – and helping patients improve their quality of life.
Seizures can happen in patients with other serious illnesses, such as kidney or liver failure, explained, Bandon Westover, MD, PhD, executive director of the Clinical Data Animation Center at MGH, but many providers simply don’t know about it.
“Right now, we mostly ignore the brain unless there’s a special need for suspicion,” he said. “In a year’s time, we’ll be catching a lot more seizures and we’ll be doing it with algorithms that can monitor patients continuously and identify more ambiguous patterns of dysfunction that can damage the brain in a similar manner to seizures.”
AUTOMATING MALARIA DETECTION IN DEVELOPING REGIONS
Malaria is a daily threat for approximately half the world’s population. Nearly half a million people died from the mosquito-borne disease in 2017, according to the World Health Organization, and the majority of the victims are children under the age of five.
Deep learning tools can automate the process of quantifying malaria parasites in blood samples, a challenging task for providers working without pathologist partners. One such tool achieved 90 percent accuracy and specificity, putting it on par with pathology experts.
This type of software can be run on a smartphone hooked up to a camera on a microscope, dramatically expanding access to expert-level diagnosis and monitoring.
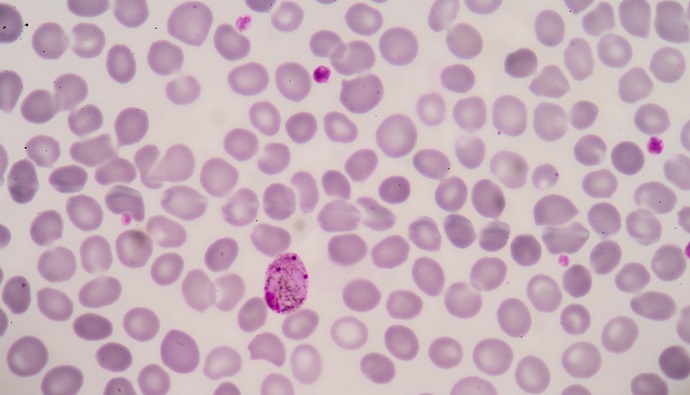
Source: Getty Images
AUGMENTING DIAGNOSTICS AND DECISION-MAKING
Artificial intelligence has made especially swift progress in diagnostic specialties, including pathology. AI will continue to speed down the road to maturity in this area, predicts Annette Kim, MD, PhD, associate professor of pathology at BWH and Harvard Medical School.
“Pathology is at the center of diagnosis, and diagnosis underpins a huge percentage of all patient care. We’re integrating a huge amount of data that funnels through us to come to a diagnosis. As the number of data points increases, it negatively impacts the time we have to synthesize the information,” she said.
AI can help automate routine, high-volume tasks, prioritize and triage cases to ensure patients are getting speedy access to the right care, and make sure that pathologists don’t miss key information hidden in the enormous volumes of clinical and test data they must comb through every day.
“This is where AI can have a huge impact on practice by allowing us to use our limited time in the most meaningful manner,” Kim stressed.
PREDICTING THE RISK OF SUICIDE AND SELF-HARM
Suicide is the tenth leading cause of death in the United States, claiming 45,000 lives in 2016. Suicide rates are on the rise due to a number of complex socioeconomic and mental health factors, and identifying patients at the highest risk of self-harm is a difficult and imprecise science.
Natural language processing and other AI methodologies may help providers identify high-risk patients earlier and more reliably. AI can comb through social media posts, electronic health record notes, and other free-text documents to flag words or concepts associated with the risk of harm.
Researchers also hope to develop AI-driven apps to provide support and therapy to individuals likely to harm themselves, especially teenagers who commit suicide at higher rates than other age groups.
Connecting patients with mental health resources before they reach a time of crisis could save thousands of lives every year.
REIMAGINING THE WORLD OF MEDICAL IMAGING
Radiology is already one of AI’s early beneficiaries, but providers are just at the beginning of what they will be able to accomplish in the next few years as machine learning explodes into the imaging realm.
AI is predicted to bring earlier detection, more accurate assessment of complex images, and less expensive testing for patients across a huge number of clinical areas.
But as leaders in the AI revolution, radiologists also have a significant responsibility to develop and deploy best practices in terms of trustworthiness, workflow, and data protection.
“We certainly feel the onus on the radiology community to make sure we do deliver and translate this into improved care,” said Alexandra Golby, MD, a neurosurgeon and radiologist at BWH and Harvard Medical School.
“Can radiology live up to the expectations? There are certainly some challenges, including trust and understanding of what the algorithms are delivering. But we desperately need it, and we want to equalize care across the world.”
Radiologists have been among the first to overcome their trepidation about the role of AI in a changing clinical world, and are eagerly embracing the possibilities of this transformative approach to augmenting human skills.”
“All of the imaging societies have opened their doors to the AI adventure,” Golby said. “The community very anxious to learn, codevelop, and work with all of the industry partners to turn this technology into truly valuable tools. We’re very optimistic and very excited, and we look forward to learning more about how AI can improve care.”

